12.-SUDDEN UNEXPECTED DEATH AT THE HOSPITAL EMERGENCY SERVICE OF AN WOMAN TREATED FOR ANXIETY NEUROSIS:HISTOPATHOLOGICAL FINDINGS.
Prof.Garfia.A
Prof.Garfia.A
Patients who suffer serious psychiatric problems, and those others whose symptoms are half way between purely emotional disorders and those dependent on somatization of psychological conflicts, make up a group of patients for whom diagnosis requires special attention and effort. The first form a group at high risk of unexpected death from illnesses so common that it is really surprising that they are not diagnosed and treated in time. The second are faced with the difficulty at diagnosis of differentiating between the truly emotional and the somatic, with the secondary danger of obviating the real somatic cause of some clinical state, with symptoms easily labelled as psychological. At times reality asserts itself drastically, and is legally conflictive for the doctor or the hospital team.
It is presented a case of unexpected death, which took place at the Medical Emergency Service, of a patient diagnosed with anxiety neurosis.
The forensic autopsy discovered the existence of a pheochromocytoma of the left adrenal gland .
Cases of sudden unexpected death associated with the tumor pathology occur seldom. Generally, tumors can causes "truly" sudden death when they provocated serious circulatories problems, such as brain haemorrhages -leucemies- or fatal haemoptisis; massive pulmonary embolization and/or tumoral pulmonary embolization ( liver and digestive system tumors); or massive carcinomatosis ( primary tumors found in the breast, digestive system, pancreas and genital organs).This tumor, the pheochromocytoma, can produce serious cardiovascular pathology, inclusive sudden death, due to the excessive producction of chemical messengers which can produce an overstimulation in the Cardiovascular System, originating a toxic nor-epinephrin myocarditis - due to a direct toxic effect on the myocardiocites; between these messengers are the Adrenalin and Nor-adrenalin and the peptide named adrenomedulin.
CASE REPORT
In this report it is presented a case of a woman, 50 years old, who was attended at the Hospital Emergency Service at 3.00 hours in the morning. She had a clinical syntomatology consisted of: abdominal pain, dyspnea, and vomiting with blood- tinged froth. The arterial pression was 12/6 and the ECG presented sinusal rythm 120 x. The woman go to the observation room and presented a little later, progressive dyspnea and the followings parameters: Ph 7.21; PCO2 33; PO2 50; HCO3- 13; and O2 saturation 77%. Posteriorly,the woman presented two episodes of cardiac arrest, being necessary aplication of avanced RCP. The patient was transported to the Unit Care and connected to assisted ventilation; in that moment, the arterial pression was 60/0, the ECG shows a sinusal rythms to 130x', a Glasgow of 3 and arreactive mydriasis. Two hours later the patient was pronounced dead. A clinical diagnosis of cardiogenic shock and pulmonary edema of cardiogenic origin was emitted.The family solicited a legal autopsy.
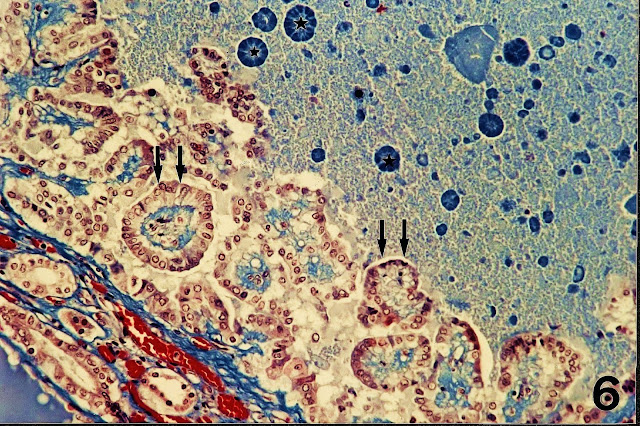
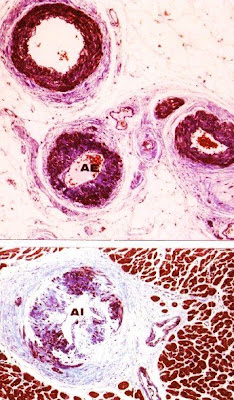
The macroscopic examination demonstrated the existence of a tumor located in the left renal fossa of 8x5x4,5 cm of maximal diameters (Foto nº 1). Both kidneys were normal.The lungs showed pulmonary edema, and the rest of the organs were normal. Microscopically the epicardial and intramural arterioles in the heart showed hypertensive changes (see Foto nº 2) and also the renal arterioles. The tumor was rounded for a capsule of conective tissue but we can found some tumoral cells penetrating the capsule.Tumor cells were polygonals and they had an ample cytoplasm, brownish, occupied by acidophile granulations.The nuclei were rounded and sometimes giant and pleomorphic. Inside the tumor we found some ganglionar cells and also nests of the glomerulous cells of the adrenal gland ( see Fotos 4-5). The heart shows very abundant focus of myocardiocites presenting contraction band necrosis which do not show a coronary distribution pattern dependence. A diagnostic of epinephrine myocarditis (focal myocarditis) was emitted and was considered the cause of death.
The macroscopic examination demonstrated the existence of a tumor located in the left renal fossa of 8x5x4,5 cm of maximal diameters (Foto nº 1). Both kidneys were normal.The lungs showed pulmonary edema, and the rest of the organs were normal. Microscopically the epicardial and intramural arterioles in the heart showed hypertensive changes (see Foto nº 2) and also the renal arterioles. The tumor was rounded for a capsule of conective tissue but we can found some tumoral cells penetrating the capsule.Tumor cells were polygonals and they had an ample cytoplasm, brownish, occupied by acidophile granulations.The nuclei were rounded and sometimes giant and pleomorphic. Inside the tumor we found some ganglionar cells and also nests of the glomerulous cells of the adrenal gland ( see Fotos 4-5). The heart shows very abundant focus of myocardiocites presenting contraction band necrosis which do not show a coronary distribution pattern dependence. A diagnostic of epinephrine myocarditis (focal myocarditis) was emitted and was considered the cause of death.
 |
| PROF. GARFIA.A BLOG 12 FORENSICPATHOLOGYFORUM |
 |
| PROF. GARFIA.A BLOG 13 FORENSICPATHOLOGYFORUM |
 |
| PROF. GARFIA.A BLOG 13 FORENSICPATHOLOGYFORUM |
Prof.Garfia.A
 |
| PROF. GARFIA.A BLOG 13 FORENSICPATHOLOGYFORUM |
 |
| PROF. GARFIA.A BLOG 13 FORENSICPATHOLOGYFORUM |
Fig.5.- Nest of tumoral and ganglionar cells inside the tumor. Arrows showing rests of glomerulous cells of the adrenal gland. Prof.Garfia.A
REFERENCES
1. Garfia A, Borondo J.- Muerte súbita en Patología Forense. Rev Esp Med Legal.Enero-Junio 1989; pp. 31-43.
2. Garfia A.- Glomus tissue in the vicinity of the human carotid sinus. Journal of Anatomy 130: 1-12 (1980).
3.- Garfia A.- En Böck, P.- The Paraganglia. Handbuch der mikroskopischen Anatomie. Band 6. Blutgefäß- und Lymphgefäßapparat. 8 Teil.Springer-Verlag. Berlin1982. pp.89.
4.- Garfia A.- Muerte Súbita o Retardada asociada a la Patología del Compartimento Lateral del cuello: el papel fisiopatológico de los Barorreceptores del Seno Carotídeo y de los Quimiorreceprores del Glomus Caroticum. Cuad Med For 16-17. 1999. 85-153
5.-Garfia et al.-Vascular lesions in the intestinal ischaemia induced by Cocaine-Alcohol Abuse:Report of a Fatal Case due to Overdose.Journal of Forensic Science.Vol 35.nº 3.1990
6. Henle J.- Allgemeine Anatomie. Leipzig 1841.
7. Henle J.- Über die Gewebe der Nebenniere und Hypophyse. Z rat Med 24, 143-152 (1865).
8. Rosai J.- Ackerman´s Surgical Pathology. 7ª Ed. Ed Mosby C. Washington D.C. 1989.
9. Cotran R, Kumar V, Robbins S.- Pathological Basis of Disease. Interamericana. 1995.
10. Silver MD, Gotlieb AI, Schoen FJ.- Cardiovascular Pathology. Churchill Livingstone.N.Y. 2001.
11. Karch SB .- The Pathology of Drug Abuse. 3ª Ed. CRC Press. 2002. pp. 104.
12. Szakacs, J and Cannon, A.- L-Norepinephrine myocarditis. Am J Clin Pathol. 30, pp. 425-434.
13. Van Vliet, Burchell HB, Titus JL.- Focal myocarditis associated with pheochromocytoma. N Engl J Med 274:1102-1105. 1966.
14. Jessurun CR, Adam K, Moisek J Jr, Wilansky S.- Pheochromocytoma-induced myocardial infarction in pregnancy. Tex Heart Inst J 20:120-124;1993.
15. Morris K, McDevitt B.- Pheochromocytoma presenting as a case of mesenteric vascular occlusion. Ir Med J 78:356-358.1985.
16. Gulliford MC, Hawkins CP, Murphy RP.- Spontaneous dissection of the carotid artery and pheochromocytoma. Br J HospMed 35: 416-420, 1986.
17. DeSouza TG, Berlad L, Shaphiro K et al.,- Pheochromocytoma and multiple intracerebral aneurysms. J Pediatr 108: 947-950. 1986.
 measured 1 cm long and orientated parallel to the aortic cusps of the aortic valve which penetrated through the aortic wall
measured 1 cm long and orientated parallel to the aortic cusps of the aortic valve which penetrated through the aortic wall